Effectiveness of hemostatic agents in thyroid surgery for the prevention of postoperative bleeding from freeamfva's blog
Effectiveness of hemostatic agents in thyroid surgery for the prevention of postoperative bleeding
Postoperative bleeding remains one of the most frequent, but rarely life-threatening complications in thyroid surgery. Although arterial bleeding is the main cause of postoperative hemorrhage, most often no actively bleeding vessel can be found during revision. Therefore, the coagulation technique for larger vessels may play a minor role, and hemostatic agents could be of higher importance. In this descriptive, retrospective study, data of 279 patients with thyroid surgery (total of 414 thyroid lobectomies) were collected. We reviewed the electronic medical record by analyzing the histological, operative, laboratory and discharge reports in regards to postoperative bleeding. Of the 414 operated thyroid lobes, 2.4% (n = 10) bled. 1.4% (n = 6) needed reoperation while the other 1.0% (n = 4) could be treated conservatively. Hemostatic patches were applied 286 (69.1%) times. Of the 128 (30.9%) patch-free operated sides, 4.7% (n = 6) suffered postoperative bleeding. Tachosil® alone was used 211 (51.0%) times and bleeding occurred in 1.4% (n = 3). Without statistical significance (p = 0.08) the use of Tachosil® seems to help preventing postoperative bleeding. The combination with other patches doesn’t appear to be more efficient.To get more news abouthemostasis, you can visit rusuntacmed.com official website.
Due to its endocrine function, the thyroid gland is a well perfused organ. For this reason, a good hemostasis during surgical procedures is of utmost importance. Postoperative bleeding remains one of the most frequent complications, and can cause airway compression and respiratory distress in severe cases. Moreover, intraoperative bleeding can obscure important structures like the parathyroid glands and the recurrent laryngeal nerve, complicating surgical dissection and increasing morbidity Aleksandar, et al.1,2,3. The frequency of postoperative cervical hematoma (PCH) in thyroid surgery requiring reoperation ranges from 0 to 9.1%4, and it is the most common reason for return to the operating room5.
Many factors influence perioperative hemostasis. In the literature, several preoperative patient’s risk factors are described, such as Grave’s disease6,7,8,9, benign pathology6,8,9, the use of anticoagulation or antiplatelet medication while doing surgery6,10, an increased size of the pathology specimen6, an emergent admission8, presence of 2 or more comorbidities8, previous thyroid surgery9, age 65 years and older7,11, African-American race7 and history of alcohol abuse7. A BMI greater than 30 kg/m2 11,12 and male sex7,9,11 are also independent risk factors associated with PCH. Furthermore, postoperative hypertension increases the risk of postoperative bleeding9,13.
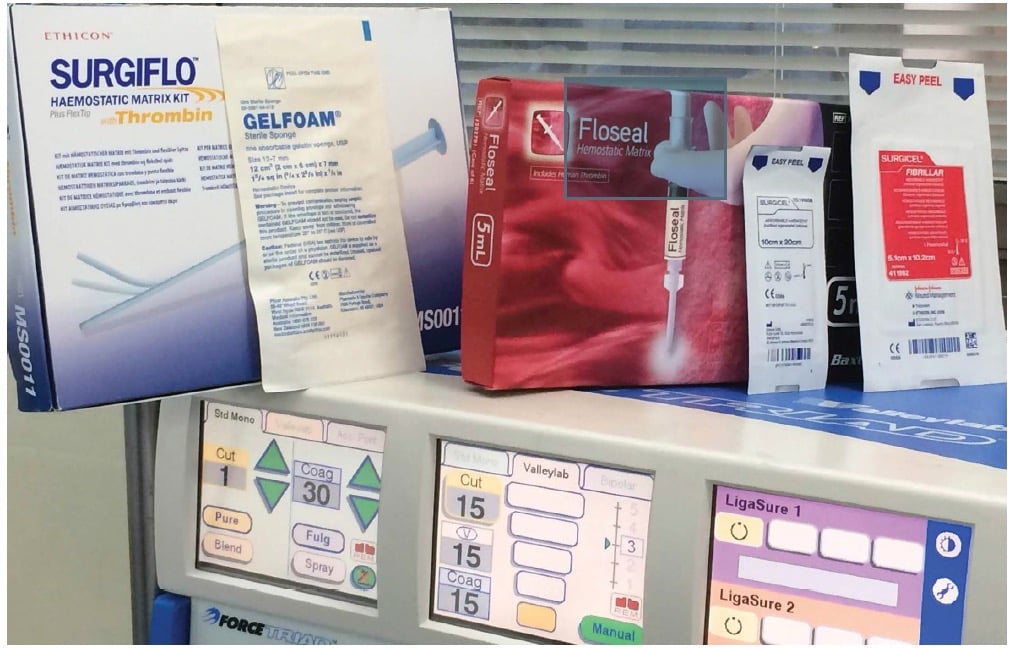
In the past century, the only instruments at a surgeon’s disposal to obliterate vessels were needle and thread in order to create a ligation. Nowadays, the industry provides a variety of devices to seal and cut vessels, such as metal clips, bipolar coagulation forceps (e.g. BiClamp®) and ultrasound scissors. The type of sealing technique doesn’t seem to affect the risk of postoperative bleeding. Alesina et al. and Brzezinski et al. found no difference in complication rate by using BiClamp® or ligations in their studies. Other vessel sealing systems, like LigaSure® and Harmonic Scalpel® have proven to be efficient in safely sealing the vessels with minimal thermal effect on the surrounding tissue, but they are expensive and only meant for a single use14,15. On the other hand, many studies such as the one from McNally et al. showed no difference in comparing ultrasonic dissection devices (Harmonic Focus®) with electronic vessel sealing systems (LigaSure®) in several criteria except from operating time, which was shorter for ultrasonic devices16.
Although arterial bleeding is the main cause of postoperative hemorrhage, as it starts earlier than venous oozing. Most often no actively bleeding vessel can be found during reoperation12. Therefore, the coagulation technique for the larger vessel may play a minor role. As certain conditions, like for example the need of anticoagulant agents cannot be changed for different reasons, hemostatic agents may play an important role. Therefore, we focused on sealant patches.
Basically, there are two main categories of hemostatic patches available: biologically active and physical agents. The first group consists of sealant matrixes containing human coagulation factors as a coating on the surface. In contact with body fluids, such as blood, the components of the coating diffuse into the wound activating the fibrinogen-thrombin reaction, thus initiating the last phase of the human coagulation cascade. This process leads to the formation of a fibrin clot, which holds the collagen matrix to the wound surface, creating a mechanically stable network that provides sealing. Among the commercially available products are Surgiflo®, Floseal® (gelatin-thrombin matrix sealants), Evarrest® and Tachosil® (fibrinogen and thrombin coated matrix), the latter being most frequently used at the University Hospital of Basel (USB). The second group consists of physical agents that enhance hemostasis using a passive substrate. An oxidized cellulose patch, when saturated with blood, provides a surface for platelet adhesion and aggregation, thus initiating the formation of a durable clot that doesn’t wash away or bleed again when irrigated. Tabotamp Snow®, Spongostan™ and Nu-Knit® are examples that belong to this type of physical agents.
Post
| By | freeamfva |
| Added | Sep 22 '22 |
Tags
Rate
Archives
- All
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
The Wall